Contributed by Shveta S. Motwani MD, T. Douglas Bradley MD, FRCPC
A 35 year old gentleman was referred for suspicion of obstructive sleep apnea (OSA). His past medical history included two episodes of stroke at ages 27 and 34 years with no residual neurological deficits in association with a patent foramen ovale which was surgically closed 6 months prior to the visit to our clinic. His sleep history included snoring, witnessed apneas and spontaneous arousals described by his wife with no difficulty in resuming sleep. He described feeling fatigued and sleepy in the mornings. His Epworth Sleepiness Score was 9 and Mallampati score was 2.
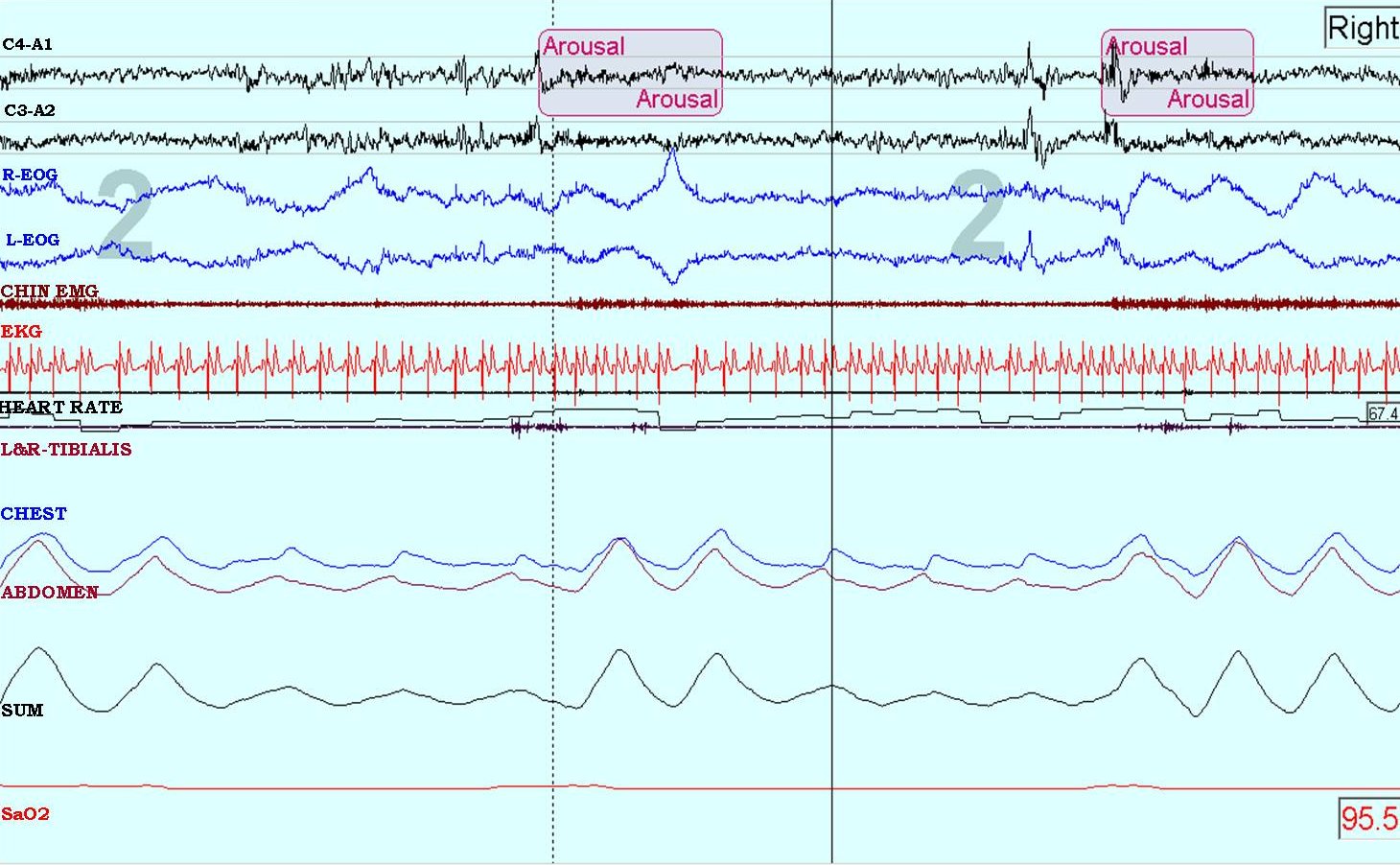
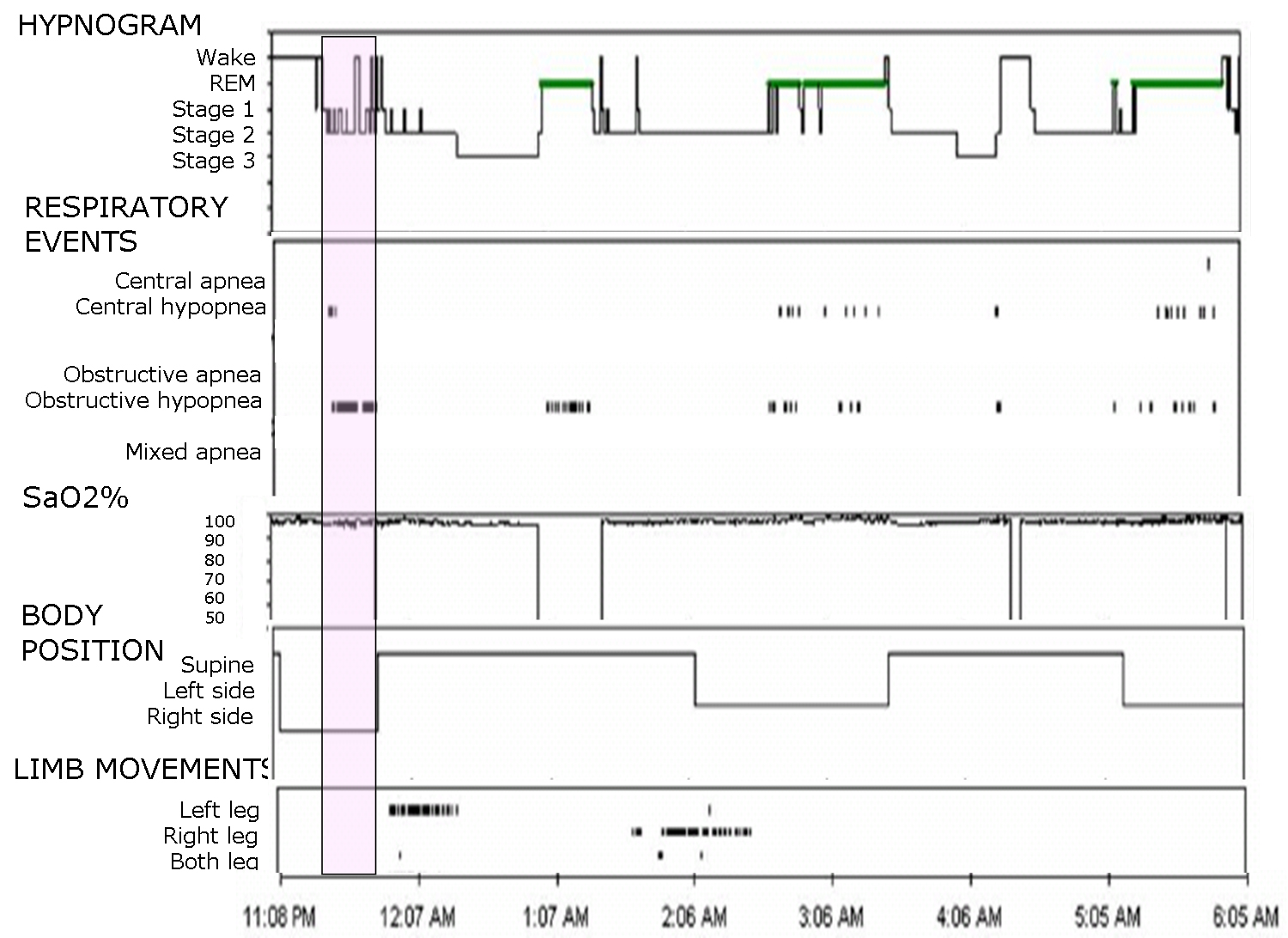
A diagnostic sleep study showed a mild obstructive sleep apnea with an overall apnea-hypopnea index (AHI) of 14.4 events/hr and mild periodic limb movements during sleep with an index of 14.1 events/hr. Interestingly, when he was in the right lateral position, his AHI was 87 events/hr compared to only 17 events/hr on the left side and 6 events/hr while supine. He spent 22 minutes on his right side all of which was spent in stages N1 and N2 sleep. The figure below shows an epoch from the polysomnogram (PSG) recording demonstrating 2 obstructive hypopneas as indicated by the out-of-phase chest and abdominal movements on respiratory inductance plethysmography, accompanied by arousals from sleep while in the right lateral position.
- What possible explanation might there be for this right lateral positional OSA?
- What would you think of looking for on the physical examination when presented with this case?
- Unilateral nasal obstruction.
- Left-sided nasal septal deviation.
OSA presenting in the right or left lateral decubitus position suggests the possibility of unilateral nasal obstruction. Deviated nasal septum (DNS), nasal polyps, inferior turbinate hypertrophy, large nasopharyngeal masses, chronic allergic or non-allergic nasal congestion are some causes that should be considered. This relates to the phenomenon of the “nasal cycle” and the effect of posture on nasal resistance. This was first described in the ancient Hindu literature by Yoga practitioners in the Vedic period approximately 3000 years ago1, 3. It was later described in modern scientific literature by Kayser2.
The nasal cycle refers to spontaneous and reciprocal changes in unilateral nasal airflow associated with congestion and decongestion of the nasal venous sinuses that occurs approximately every 0.5 to 3 hours. As the nasal resistance increases in one nostril, it decreases in the other, although the total collective nasal resistance through both nostrils remains constant. Total nasal resistance is regulated by the sympathetic nervous system.
In addition, airflow resistance of the two nostrils can be influenced asymmetrically by proprioceptive stimulation of the side of the body, specifically the axilla and hips3. Thus, pressure applied on one side of the body causes ipsilateral nasal venous congestion with increased nasal resistance (decreased airflow) and contralateral decongestion with decreased nasal resistance (increased airflow). For example, when an individual lies down in the right lateral position, there is a fall in resistance with an increase in airflow through the left nostril that ensures dominant flow through the upper nostril3. Since this patient’s OSA occurred predominantly in the right lateral position, this suggests an abnormality in the airflow through the left nostril, which was limited by a left sided nasal septal deviation. Simultaneously, the right nasal passage was probably constricted due to the nasal reflex. Such nasal obstruction leads to an elevation in the upstream airflow resistance which increases the negative collapsing pressure that renders the pharynx more susceptible to collapse and therefore, to OSA4.
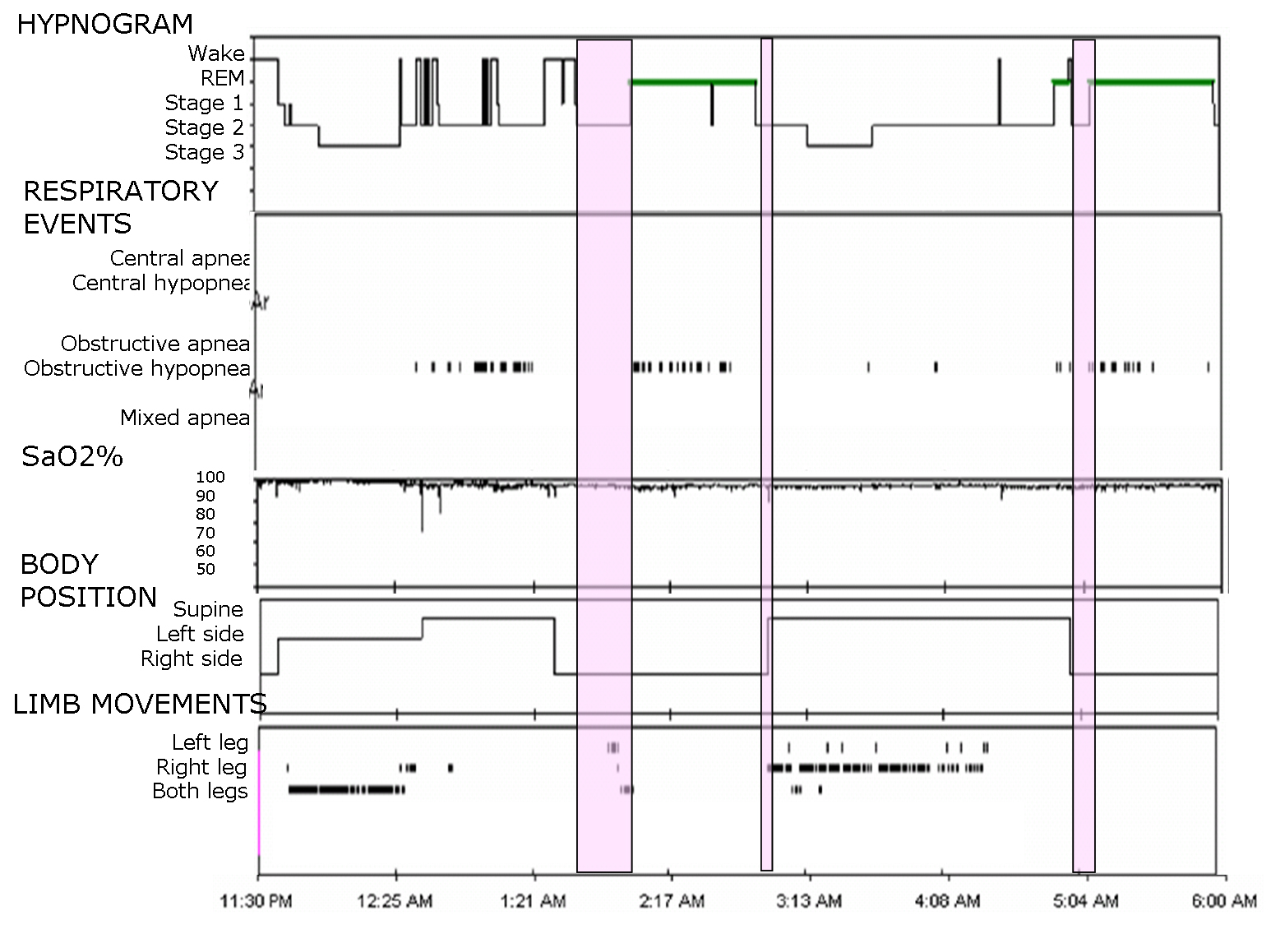
We referred our patient to an otolaryngologist for assessment and repair of his deviated nasal septum. A nasal septoplasty was performed following which a PSG was repeated. The patient reported a marked improvement in nasal breathing after the surgery in association with a profound reduction in the non-REM AHI in the right decubitus position from 87.3 to 1.6. His overall AHI, however, decreased only modestly from 14.4 to 10.2.
Figures 2 and 3 show composite hypnograms before and after surgery with highlighted portions of non-REM sleep on the right side.
A recent randomized controlled trial of nasal surgery for fixed nasal obstruction in OSA patients found nasal surgery to be effective (defined by the authors as post-operative AHI <15/hour along with ≥ 50% decrease in AHI from the baseline) in about 15% patients in the treatment group. This study did not stratify AHI in different body positions.5, 6 It has also been shown in some instances to lower CPAP requirements 7 and improve compliance with CPAP.
Some limitations apply to the observations made from this case study. On the diagnostic sleep study, he spent only 22 minutes in the right lateral position so that the severity of OSA in that position may have been over-estimated. Nasal pressure was not measured during the diagnostic sleep study and obstructive apneas and hypopneas were scored on the basis of out-of-phase thoracoabdominal motion on respiratory inductance plethysmography according to standard criteria 7. Nasal resistance was not measured before and after nasal surgery so we could not prove that nasal resistance diminished following septoplasty.
In summary, this case highlights a possible anatomical abnormality contributing to the pathogenesis of OSA in the right lateral position that improved following correction of nasal septal deviation. Nasal surgery has not been shown to consistently alleviate OSA in patients who experience a reduction in nasal resistance following septoplasty. Therefore, in general, the role of nasal obstruction and nasal surgery for treatment of OSA remains controversial. This controversy would best be resolved by larger randomized controlled trials.8, 9 Nevertheless, the present case points to a possible role of unilateral nasal obstruction in the causation of lateral-positional OSA, since correction of the deviated septum was accompanied by alleviation of OSA in the right lateral position. In addition, there does not appear to be an alternative explanation for our findings in this regard, and no literature to elucidate other causative factors for lateral positional OSA.
References:
- Sen H. Observations on the alternate erectility of the nasal mucous membrane. Lancet 1901; 1: 564.
- Kayser R. Die exacte messung der luftdurchgangigkeit der nase. Arch Laryngol Rhinol 1895; 3: 101–20
- Eccles, R. Nasal airflow in health and disease. Acta Otolaryngol 2000; 120: 580–595.
- Ryan CM, Bradley TD. Pathogenesis of Obstructive sleep apnea. J Appl Physiol. 2005 Dec;99(6):2440-50.
- Koutsourelakis I, Georgoulopoulos G, Perraki E, Vagiakis E, Roussos C and Zakynthinos SG. Randomised trial of nasal surgery for fixed nasal obstruction in obstructive sleep apnoea. Eur Respir J. 2008 Jan;31(1):110-7.
- Friedman M, Tanyeri H, Lim JW, Landsberg R, Vaidyanathan K, Caldarelli D. Effect of improved nasal breating on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000 Jan;122(1):71-4.
- Iber C, Ancoli-Israel S, Chesson A, Quan SF. for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Westchester: American Academy of Sleep Medicine; 2007.
- Kohler M, Bloch KE, Stradling JR. The role of nose in the pathogenesis of obstructive sleep apnoea and snoring Eur Respir J 2007; 30: 1208-1215.
- Kohler M, Bloch KE, Stradling JR. The role of the nose in the pathogenesis of obstructive sleep apnea. Curr Opin Otolaryngol Head Neck Surg 2009 17:33–37