Contributed by Klar Yaggi, M.D., M.P.H and Shahrokh Javaheri M.D.
Identify and describe the abnormality in the accompanying 10 minute polysomnogram fragment below. What medication is associated with this abnormality?
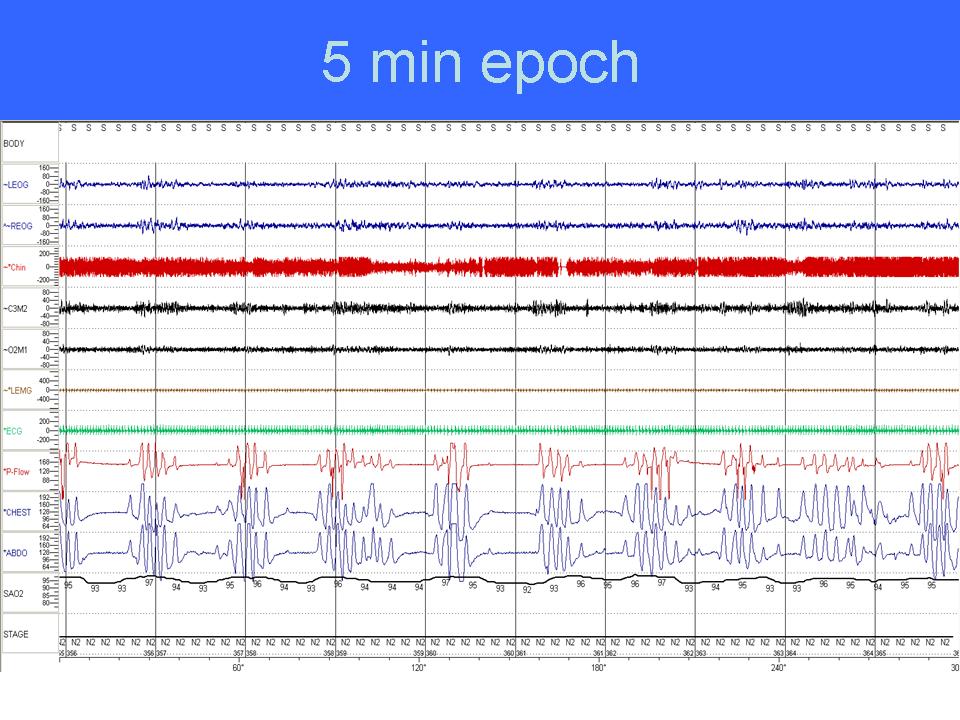
This is a 5-minute polysomnogram fragment from a patient in stage N2 sleep on chronic treatment with 55mg daily, morphine equivalent for chronic low back pain, revealing an ataxic breathing pattern associated with intermittent oxygen desaturations and arousals.
Discussion: This is a 5-minute polysomnogram fragment from a patient in stage N2 sleep on chronic opioid medication revealing an ataxic breathing pattern associated with intermittent oxygen desaturations. Note that the breathing pattern has variation in depth and rate with frequent pauses largely in the form of central and obstructive disordered breathing events. This breathing pattern with irregular variation in depth and frequency has been previously described by Biot in 1876 and is referred to as “Biot’s respiration” (1). Please note that the disordered breathing events observed with Biot’s respiration are characteristically short. This is in contrast to Hunter-Cheyne –Stokes breathing (Hunter was the first physician who described this pattern of breathing), which is frequently observed in systolic heart failure and is characterized by prolonged crescendo/decrescendo changes in tidal volume (2).
Ataxic breathing is associated with chronic opioid use. In the last decade, there has been a major change in the management of chronic pain with a major increase in the therapeutic use of opioids. Although there appears to be respiratory tolerance (i.e. absent to mild respiratory depression) during wakefulness with chronic opioid, profound respiratory depression characterized by various forms of sleep disordered breathing and hypoventilation occur during sleep. Walker and colleagues(3) performed polysomnography in a cohort of 60 patients taking opioids for pain management. These patients were matched with 60 control patients not taking opioids for age, gender, and BMI. Chronic opioid use was associated with a significantly higher apnea hypopnea index in a dose response fashion (largely due to central apneas) and a lower oxygen saturation. The adverse health consequences associated with this pattern remains to be determined. Given that chronic narcotic use has been associated with sudden death in some cases; further work regarding the impact of this breathing pattern is required.
This pattern of breathing is resistant to CPAP therapy, but improves considerably with appropriate titration with new pressure support servoventilators (4). Nocturnal oxygen therapy, theophylline and acetazolamide which have been used for treatment of central sleep apnea in heart failure (5) have not been studied systematically in opioid-associated sleep disordered breathing. We suspect that these modalities may improve the central but not the obstructive component of disordered breathing due to opioids. Dose reduction or discontinuation of opioid medication would be expected to either mitigate or even eliminate sleep-related breathing disorders.
References:
- Biot, MC. Contribution a l’ètude de phènomène respiratoire de Cheyne-Stokes. Lyon Mèd1876;23:517-28,561-7.
- Dowdell WT, Javaheri S, McGinnis W. Cheyne-Stokes respiration presenting as sleep apnea syndrome: Clinical and polysomnographic features. Am Rev Respir Dis 1990;141:871-879
- Walker M, Farney J, et al. Chronic opioid use a risk factor for the development of central sleep apnea and ataxic breathing. J Clin Sleep Med 2007;3:455-61.
- Javaheri S, Malik A, Smith J and Chung J. Adaptive pressure support servo-ventilation: a novel treatment for sleep apnea associated with use of opioids. J Clin Sleep Med 2008; 4:305-310
- Javaheri S. Heart failure. In: Principles and Practices of Sleep Medicine, 4/e; Edited by Kryger MH, Roth T, Dement WC; WB Saunders, Philadelphia 2010.