Contributed by Malcolm Kohler, MD and Konrad E. Bloch, MD, Sleep Disorders Centre and Pulmonary Division, University Hospital of Zurich, Switzerl
The parents of a 25 year old physically impaired man with a BMI of 29 kg/m2observed occasional apneas during sleep but no snoring or choking. The patient feels unrefreshed in the morning despite adequate sleep duration.
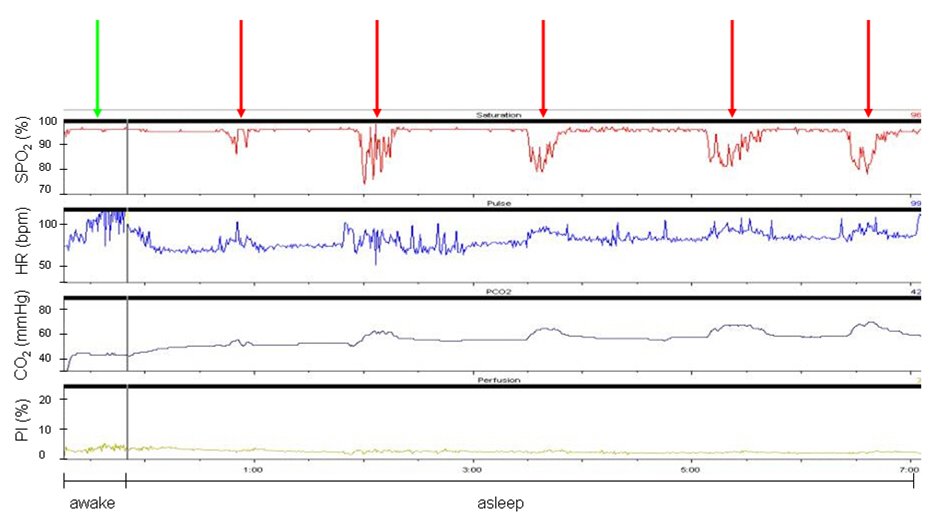
Shown is a seven hour overnight recording of arterial oxygen saturation (SpO2), heart rate (HR), transcutaneous carbon dioxide tension (PtcCO2) and the perfusion index (PI, the ratio between the pulsatile and the nonpulsatile components of the infrared signal corresponding to the pulsatile and the nonpulsatile amounts of blood as a measure of skin perfusion) of the combined ear lobe sensor.
Question: What does the sleep study show and what is the patients‘ underlying medical disorder?
During wakefulness, oxygen saturation and carbon dioxide levels (PtcCO2) were at normal levels and heart rate was slightly elevated (green arrow). Over the course of the night there are 5 discrete periods of marked oxygen desaturation associated with increases in heart rate and transient elevations in PtcCO2 (red arrows). Note the progressive increase in PtcCO2 from the beginning (43 mmHg) to the end of the recording (62 mmHg).
The patient has been diagnosed in his childhood with Duchenne muscular dystrophy (DMD) and has been wheelchair-bound since age 15. His current forced vital capacity and maximal inspiratory/expiratory pressures are markedly reduced (28%, 24% and 12% predicted).
The findings of the sleep study and the history of DMD lead to the diagnosis of muscular dystrophy-associated hypoventilation. The pattern of periodic oxygen desaturations associated with increases in PtcCO2 are highly suggestive for REM-sleep associated phases of hypoventilation. The underlying mechanisms of REM-sleep associated hypoventilation are thought to be related to inhibition of respiratory muscle tonic and phasic activity, reduction in respiratory drive, blunting of chemosensitivity and increase in upper airway resistance.
In more advanced stages of DMD, the progressive spinal and chest wall deformity and impairment of respiratory muscle function leads to hypercapnic respiratory failure. Typical daytime symptoms are morning headaches, unrefreshing sleep and excessive daytime sleepiness. Therapy of hypoventilation syndrome consists of bilevel positive airway pressure treatment most often applied by nasal masks. Data of a recently published prospective cohort study in patients with DMD have shown that mean age at the beginning of mechanical ventilation was 19.8 years (range 14–31) and mean FVC was 0.73 litre (20 % of predicted) [1]. The findings of recent studies [1,2] suggest that non-invasive positive pressure ventilation and other supportive measures prolong survival of patients with DMD well into adulthood, the estimated probability of survival to age 30 years is now approximately 85%. The indication for starting ventilation in these patients usually requires both daytime symptoms and proven hypercapnic respiratory failure (increasing hypercapnia during the course of a sleep study or awake hypercapnia in an arterial blood gas analysis). Although patients with advanced DMD are highly physically impaired and ventilator-dependent most of them report preserved health related quality of life.
References:
- Disability and survival in Duchenne muscular dystrophy. Kohler M, Clarenbach CF, Bahler C, Brack T, Russi EW, Bloch KE. J Neurol Neurosurg Psychiatry 2009;80:320-325.
- Quality of life, physical disability, and respiratory impairment in Duchenne muscular dystrophy. Kohler M, Clarenbach CF, Bohni L, Brack T, Russi EW, Bloch KE. Am J Respir Crit Care Med 2005;172:1032-1036.