Contributed by Eric M. Davis, MD1 and David M. Raizen, MD, PhD1,2 1 Perelman School of Medicine at the University of Pennsylvania Division of Sleep Medicine Department of Medicine 3624 Market Street, Suite 205 Philadelphia, PA 19104, USA 2 Perelman School of Medicine at the University of Pennsylvania Department of Neurology 462 Stemmler Hall 415 Curie Boulevard Philadelphia, PA 19104, USA Corresponding Author: Eric M. Davis, MD email: emd.davis@gmail.com Statement of Contributions: EMD and DMR evaluated the patient in the hospital, interpreted the sleep study, and wrote this report. Sources of Support: None Disclaimers: None Running Head: Prolonging apneas in a hospitalized patient MESH Browser: sleep apnea, obstructive; hypercapnia, carotid body
In Brief
A type III unattended sleep study performed on an 85 year-old man during his inpatient hospitalization following cardiac arrest reveals an increase in the average apnea length from 27.9 to 52.2 seconds after a routine therapy is initiated. The longest apnea following the intervention is 205.4 seconds. By demonstrating an adverse impact of a medical intervention, this case highlights the potential benefits and risks of a routine medical therapy.
Case Vignette
An 85 year-old man with a history of ischemic cardiomyopathy presented to the hospital after a cardiac arrest while exercising. Cardiopulmonary resuscitation resulted in a return of spontaneous circulation and the patient remained neurologically intact after his arrest. He was admitted for workup and treatment.
He underwent a cardiac ventricular tachycardia (VT) ablation on hospital day two during which time he received remifentanil 3 mg, propofol 50 mg, and diphenhydramine 50 mg. Six hours following the procedure he experienced episodic oxyhemoglobin desaturations to 40-50% during sleep. A sleep consultation was requested.
Further history revealed that he snored loudly and had witnessed apneas. He slept approximately 8 hours per night and denied excessive sleepiness. On physical examination, he was normotensive; heart rate was paced at 80/minute; respiratory rate was 12/minute; and oxyhemoglobin saturation was 97% on room air. His body mass index was 24 kg/m2. Oropharyngeal exam was notable for a modified Mallampati class IV airway and lateral pharyngeal narrowing. His lungs were clear to auscultation and heart rhythm was regular with an apical murmur. There was no peripheral edema. Neurological exam was normal.
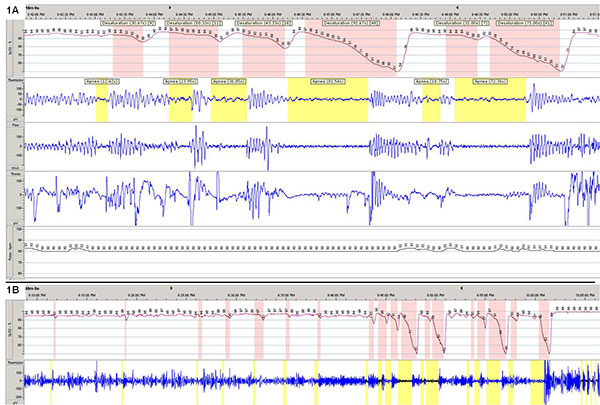
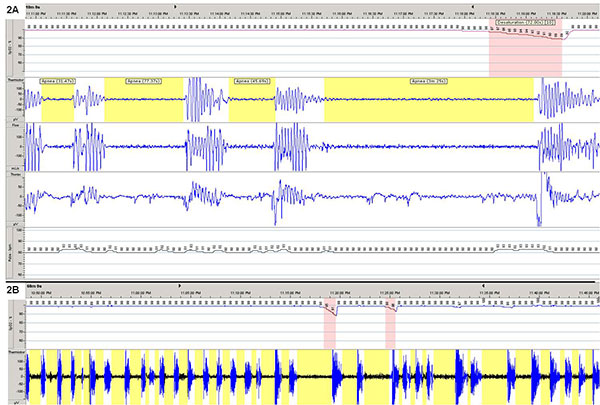
A type III unattended sleep study was performed the following night, 36 hours after his cardiac procedure (no sedating medications had been given in the interim). Representative 10-minute and 60-minute tracings are shown from the first half (Figure 1) and second half (Figure 2) of the night.
Question
What intervention did the patient receive between the two tracings?
Answer
The patient was started on supplemental oxygen therapy at 2 L/min by ward personnel in response to low SaO2 values.
Discussion
Sleep Study Interpretation
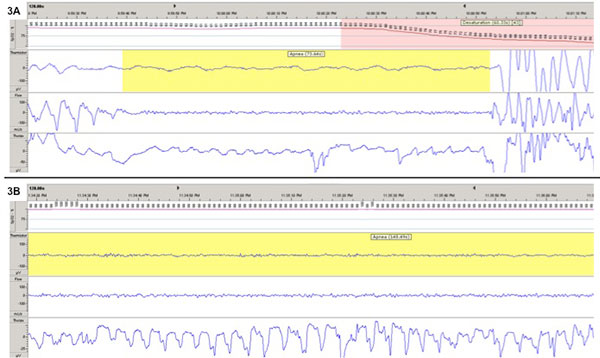
The sleep study showed an overall apnea-hypopnea index (AHI) of 28.6 events per hour with an oxygen desaturation nadir of 50.0%. The apneas appeared to be primarily obstructive or mixed events (see Figure 3). Oxygen administration led to an improvement in oxygenation (reduction from 7.9 to 0.2% of the night with a saturation below 90%) but was associated with an increase in the mean apnea duration from 27.9 to 52.2 seconds, with the longest recorded apnea of 205.4 seconds.
Discussion
Obstructive sleep apnea (OSA) is characterized by repetitive upper airway collapse during sleep which leads to sleep fragmentation, and is associated with adverse clinical outcomes (1). Arousals are often essential for reestablishing airflow. The mechanisms of arousal are thought to be three-fold: a response to a) hypercapnia, b) hypoxemia, and c) increasing negative intrapleural pressures (2). Gleeson and colleagues demonstrated that arousals are triggered most consistently by an increased effort to breathe, yet all three factors contribute (3, 4).
In the case of our patient, the nearly two-fold increase in apnea duration following the addition of supplemental oxygen suggests a relative dependence on hypoxemia to arouse during an apnea. The recent use of sedating medications may have altered the hypercapnic response and contributed to apnea prolongation although daily serum bicarbonate levels remained in the normal range throughout the testing period.
The case highlights the potential harms of empiric oxygen administration, particularly if underlying OSA is suspected. Although we did not confirm increased carbon dioxide retention, it is plausible that hypercapnia would worsen in the setting of increased apnea duration. Alford and colleagues tested this hypothesis by administering nocturnal supplemental oxygen to patients with OSA and chronic obstructive pulmonary disease. With the expected increase in apnea length (25.7 to 31.4 seconds), the end-apneic PaCO2 increased from 52 to 62 mm Hg (5).
Conversely, supplemental oxygen may indeed be helpful in select patients with OSA. Wellman and colleagues showed that subjects with high loop gain (unstable ventilator control) have significant reductions in the AHI (53% vs. 8% in control subjects) despite a slight but significant increase in the apnea duration (6). Additionally, a meta-analysis was recently performed which showed a reduction in the AHI with oxygen therapy versus air; however CPAP was altogether a better treatment than supplemental oxygen in OSA patients (7). A recent study comparing nocturnal oxygen versus CPAP versus no treatment in OSA demonstrated that only CPAP produced a significant decrease in 24-hour blood pressure measurements after 12 weeks of treatment (8).
In summary, although supplemental oxygen may be beneficial in select OSA patients, prolongation of apnea length often occurs. Given the frequent use of supplemental oxygen and the high rate of undiagnosed OSA in hospitalized patients, such effects need to be considered.
Patient Follow-Up:
The patient was started on automatically-adjusting continuous positive airway pressure (CPAP) the following night. At four months follow-up, his residual AHI was 2.1, he had excellent compliance (100% of nights with usage > 4 hours), and he had improved daytime functioning.
References
- Djonlagic I, Saboisky J, Carusona A, Stickgold R, Malhotra A. Increased sleep fragmentation leads to impaired off-line consolidation of motor memories in humans. PLoS One 2012;7(3):e34106.
- Chamberlin NL. Brain circuitry mediating arousal from obstructive sleep apnea. Currin Opin Neurobiol 2013;23(5):774-9.
- Gleeson K, Zwillich CW, White DP. The influence of increasing ventilatory effort on arousal from sleep. AmRev Respir Dis 1990;142(2):295-300.
- Dempsey JA, Smith CA, Blain GM, Xie A, Gong Y, Teodorescu M. Role of central/peripheral chemoreceptors and their interdependence in the pathophysiology of sleep apnea. Adv Exp Med Biol 2012;758:343-9.
- Alford NJ, Fletcher EC, Nickeson D. Acute oxygen in patients with sleep apnea and COPD. Chest 1986;89(1):30-8.
- Wellman A, Malhotra A, Jordan AS, Stevenson KE, Gautam S, White DP. Effect of oxygen in obstructive sleep apnea: Role of loop gain. Respir Physiol Neurobiol 2008;162:144-151.
- Mehta V, Vasu TS, Phillips B, Chung F. Obstructive sleep apnea and oxygen therapy: A systematic review of the literature and meta-analysis. J Clin Sleep Med 2013;9(3):271-279.
- Gottlieb DJ, Punjabi NM, Mehra R, Patel SR, Quan SF, Babineau DC, Tracy RP, Rueschman M, Blumenthal RS, Lewis EF, Bhatt DL, Redline S. CPAP versus oxygen in obstructive sleep apnea. N Engl J Med 2014;370(24):2276-85.
Figure Legends
Figure 1: Representative 10 minute (A) and 60 minute (B) tracings obtained during the first half of the night from a type III unattended sleep study performed on a patient. Oxyhemoglobin desaturations ≥ 4% are highlighted in red. Apnea events ≥ 10 seconds are highlighted in yellow. Event durations are labeled in seconds. SpO2% = oxyhemoglobin saturation
Figure 2: Representative 10 minute (A) and 60 minute (B) tracings obtained during the second half of the night from a type III unattended sleep study performed on a patient. Oxyhemoglobin desaturations ≥ 4% are highlighted in red. Apnea events ≥ 10 seconds are highlighted in yellow. Event durations are labeled in minutes or seconds. SpO2% = oxyhemoglobin saturation
Figure 3: Typical appearance of apneas demonstrated with the type III unattended sleep study while on room air (A) and on supplemental oxygen (B) show the presence of respiratory effort (thorax channel) despite the absence of airflow (noted in the thermistor and flow channels) which is consistent with either obstructive or mixed apneas.