Contributed by Harish Rao, M.D, and Raanan Arens, M.D., Division of Respiratory and Sleep Medicine, The Children’s Hospital at Montefiore, Albert Einstein College of Medicine, Bronx, NY; Correspondence: rarens@montefiore.org
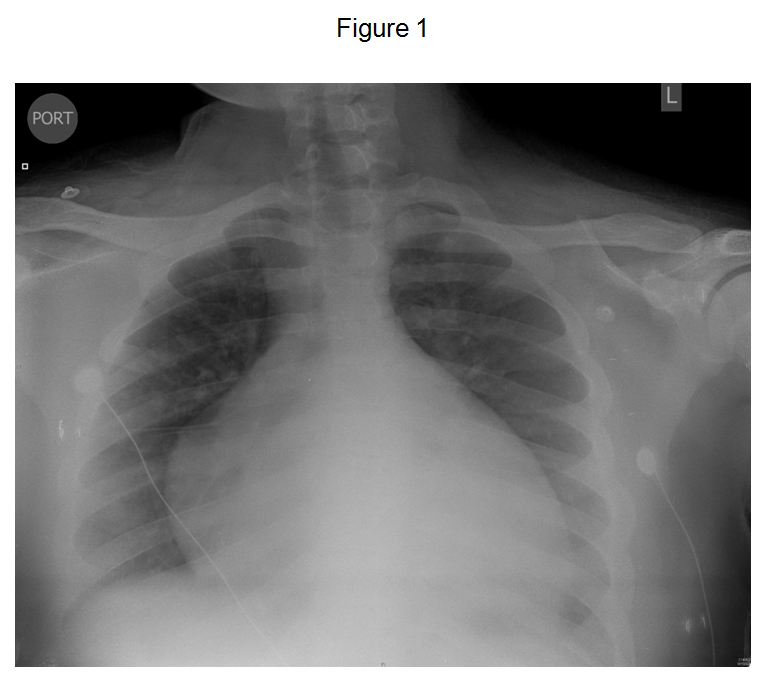
A 16 year old obese boy with a BMI of 45 kg/m2 presented to the emergency department for the first time with hemoptysis and shortness of breath lasting for one week. His admission chest x-ray is shown in Figure 1.
He was diagnosed as having idiopathic dilated cardiomyopathy and was in congestive heart failure (CHF). His ejection fraction was 18%. During the admission he was noted to have occasional apneas during sleep. His sleep history revealed snoring, but no gasping episodes or excessive daytime somnolence. A representative 2-minute epoch from the polysomnogram (PSG) is presented in Figure 2.
Legend for Figure 2
E1 & E2- EOG channels, F3 to O2- EEG channels, Chin 1 & 2 – EMG, Snore- microphone, ECG- EKG channel, LAT & RAT- actimeter, PR- pulse rate, OSAT- pulse oximetry, PTAF-nasal pressure transducer, Flow- nasal thermistor, Chest- chest plethysmography, ABD- abdomen plethysmography, Sum- sum plethysmography, Cap- capnography, ETCO2 – End tidal CO2, POS- position
Question:
- Identify the breathing pattern.
Answer:
- Cheyne-Stokes respiration with central sleep apnea (CSR-CSA)
The PSG revealed sleep efficiency of 93%, an AHI of 13.5 events/hr (mostly central apneas), and oxygen saturation nadir of 88%. Figure 3 illustrates the overnight hypnogram including: clock time, sleep stages, end-tidal CO2, SpO2, respiratory events, and arousals.
Supplemental O2 (0.5 liter/min) via nasal cannula was administrated 3 hrs after the initiation of the study (black horizontal line) and provided improvement in oxygenation and respiratory events. Recommendations included: supplemental oxygen during sleep, continued management of CHF, evaluation of the need for adenotonsillectomy, and repeat sleep study in 2 months.
Follow up
One month following the initial PSG the child developed an ischemic stroke localized to the left middle cerebral artery. He has since continued to be treated for his CHF with inotropes and diuretics, anticoagulation therapy, and supplemental oxygen during sleep. At a 3-month follow-up visit after the initial PSG he was noted to have lost 30 kg and dropped his BMI to 36 kg/m2, and a follow-up PSG demonstrated an AHI of 2.5 events/hr with few CSR-CSA events (central apnea index of 0.3 /hr). He is currently at home being treated with Milrinone infusion and is listed for cardiac transplantation.
Discussion
Sleep disordered breathing in patients with CHF is under recognized but important because it may independently predict mortality and may contribute to disease progression [1, 2].
While obstructive sleep apnea (OSA) is more common in the general population, CSR-CSA may be more common than OSA in patients with CHF [2, 3], and particularly in non-rapid eye movement (NREM) sleep, as seen in our patient.
Polysomnographic characteristics of CSR-CSA consist of central apneas with alternating hyperpneas that are associated with a waxing-waning pattern of tidal volume. A key factor that predisposes to CSR-CSA in these patients is instability of the respiratory control system characterized by a tendency to hyperventilate. Central apnea occurs when PaCO2 falls below the threshold for apnea during sleep, due to ventilatory overshoot [1].
Patients with CHF have chronic hyperventilation with eupneic PaCO2 close to the apneic threshold because of pulmonary vagal irritant receptor stimulation and increase in central and peripheral chemosensitivity. It is also proposed that these subjects have a decrease in total body stores of CO2 and O2 with resulting instability in arterial blood gas tensions in response to changes in ventilation [4].
CSR-CSA is best conceptualized as a sequence of the following events:
- In an effort to correct the hypocapnia, a hypersensitive respiratory control center initiates an apnea. This occurs when the PaCO2 is below the "apneic threshold". The PaCO2 then begins to rise.
- The duration from the beginning of the apnea until the respiratory control center detects the increasing PaCO2 is prolonged due to the increased circulatory time caused by heart failure. Although some circulatory delay is required for CSR-CSA to occur, its importance as a contributor to CSR-CSA is debated.
- Hypercapnia exists by the time the respiratory control center terminates the apnea.
- The hypercapnia then stimulates robust hyperpnea, which results in marked hypocapnia and allows the cycle of events to repeat [1].
The net effect is oscillation of ventilation between apnea and hyperpnea. Elimination of the hypocapnia with inhaled CO2, continuous positive airway pressure (CPAP), or oxygen can markedly attenuate CSR-CSA.
With respect to CSR-CSA, risk factors include male gender, advanced age, atrial fibrillation, and awake hypocapnia (PaCO2 ≤36 mmHg). CSR-CSA is observed in approximately 40% of patients with a left ventricular ejection fraction of <40% [2].
An in-laboratory overnight PSG is the gold standard diagnostic test. Treatment options for CSR-CSA include: optimization of CHF treatment, oxygen supplementation, diuretics, CPAP and cardiac resynchronization therapy [2]. As our patient responded well to oxygen therapy during the initial PSG, CPAP was not initiated.
It is also possible that obesity contributed to his respiratory pattern during sleep since he also demonstrated some obstructive events, though most of the events were central in nature. In the following months the patient had lost 30 kg and dropped his BMI to 36 kg/m2. This was attributed to the use of diuretics and a reduction in the amount of fluid retention. As stated above, the follow-up PSG showed an AHI of 2.5 with very few events of CSR-CSA.
Two conditions secondary to obesity that should be discussed in this clinical context are obesity hypoventilation syndrome (OHS) and obesity cardiomyopathy (OCMP). Obesity hypoventilation syndrome is defined as the triad of obesity, hypoventilation (PaCO2 > 45 mmHg) and sleep disordered breathing in the absence of alternative neuromuscular, mechanical or metabolic explanation for the hypoventilation [5]. Though our patient had obesity and sleep disordered breathing, he did not have hypoventilation. Obesity cardiomyopathy has been described in patients with long standing obesity leading to: left ventricular dilation, increased left ventricular wall stress, compensatory left ventricular hypertrophy, and left ventricular diastolic dysfunction. Increased age and duration of obesity are the strongest predictors of OCMP [6]. It is possible that the current subject fits the latter category although he seems younger than other reports.
Only a handful of studies describe the occurrence of CSR-CSA in children. In a recent study by Peer et al [7] evaluating both children and adults with CHF, they noted that while none of the children had CSR-CSA, 40% of the adults did exhibit it. They suggest that CSR-CSA may be an adult phenomenon. However, more studies are needed to evaluate the extent of CSR-CSA in children with CHF.
References:
-
Yumino, D. and T.D. Bradley, Central sleep apnea and Cheyne-Stokes respiration. Proc Am Thorac Soc, 2008. 5(2): p. 226-36.
-
Sharma, B., R. Owens, and A. Malhotra, Sleep in congestive heart failure. Med Clin North Am, 2010. 94(3): p. 447-64.
-
Bradley, T.D., et al., Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med, 2005. 353(19): p. 2025-33.
-
Hoch, B. and H. Barth, Cheyne-Stokes respiration as an additional risk factor for pulmonary hypertension in a boy with trisomy 21 and atrioventricular septal defect. Pediatr Pulmonol, 2001. 31(3): p. 261-4.
-
Mokhlesi, B., Obesity hypoventilation syndrome: a state-of-the-art review. Respir Care, 2010. 55(10): p. 1347-62; discussion 1363-5.
-
Dela Cruz, C.S. and R.A. Matthay, Role of obesity in cardiomyopathy and pulmonary hypertension. Clin Chest Med, 2009. 30(3): p. 509-23, ix.
-
Peer, A., et al., The occurrence of cheyne-stokes respiration in congestive heart failure: the effect of age. Front Psychiatry, 2010. 1: p. 133.