Contributed by Lavanya Kodali, MD, Vishal K. Patel, MD, and Jeremy A. Weingarten, MD, New York Methodist Hospital, Division of Pulmonary, Critical Care, and Sleep Medicine, Center for Sleep Disorders Medicine and Research, Brooklyn, New York *Corresponding author: Jeremy A. Weingarten
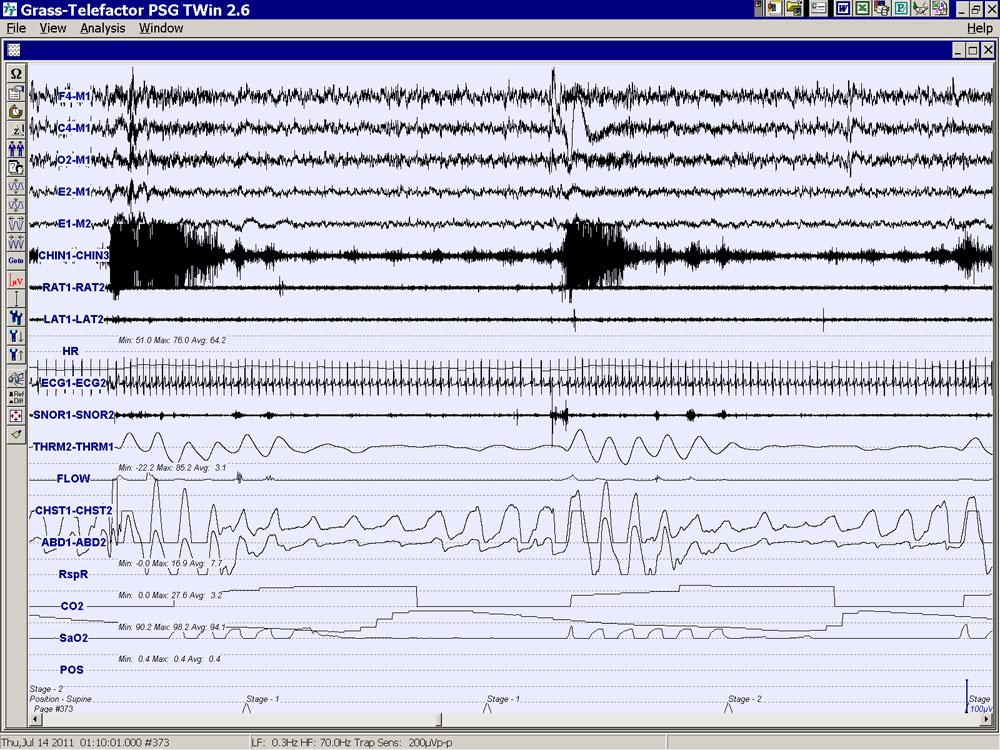
Case: A 71 year-old African American man with a body mass index (BMI) of 30 kg/m2 underwent nocturnal polysomnography (PSG) to evaluate snoring and excessive daytime sleepiness. The PSG demonstrated moderate obstructive sleep apnea (OSA) with an apnea-hypopnea index (AHI) of 15 events/hr and a nadir oxygen saturation of hemoglobin of 88%; supine AHI was 44 events/hr. Definitive obstructive events were not observed in the non-supine position, although frequent arousals associated with snoring in this position may indicate the presence of respiratory effort-related arousals (RERAs)*. The total sleep time was 337 minutes with a sleep time in the supine position of 113 minutes. A 2-minute epoch from the patient’s polysomnogram is shown in Figure 1.
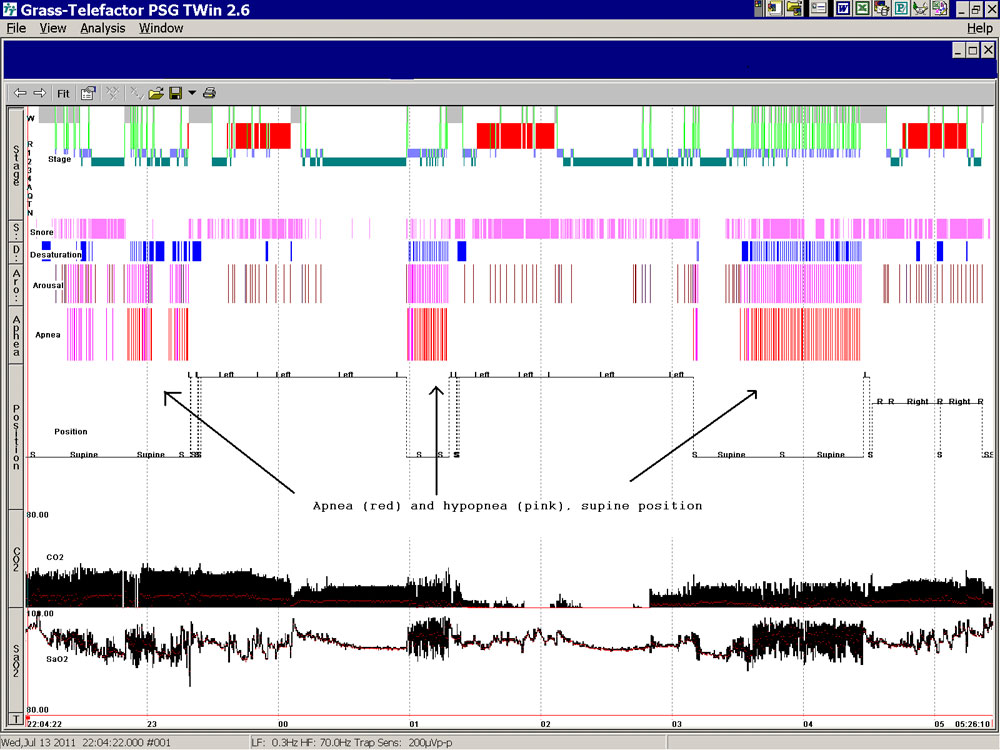
The sleep hypnogram is shown in Figure 2. Of note, rapid eye movement (REM) sleep in the supine position was not observed, which may result in an underestimation of the true severity of OSA.
Question: How would you manage sleep apnea in this individual?
A. PAP titration
B. ENT evaluation for an upper airway surgical procedure
C. Suggest an oral appliance
D. Positional therapy with avoidance of supine sleep
E. Tracheostomy
(* esophageal pressure was not measured during the study, and therefore scoring of definitive RERAs was not performed)
Answer:
A. PAP titration
Discussion: Positional OSA has been reported in up to 50% - 60% of all patients diagnosed with OSA (1). It is defined as more than a 50% reduction in AHI in the non-supine position when compared with supine sleep. Sleep position can affect the size and patency of the upper airway, resulting in an increase in the number of obstructive events in the supine position; although several physiologic mechanisms likely account for this finding, changes in upper airway dimension due to gravitational effects on the retropalatal and retroglossal airways (2) is the easiest mechanism to conceptualize. In general, individuals more likely to have positional OSA and respond well to positional therapy are younger, have a lower AHI, and are less obese (3). Although positional therapy, consisting of various methods that prevent the patient from sleeping in the supine position (the “tennis-ball” technique, positional pillows, etc.), has been studied and shown to be effective, the studies have been limited by small number of subjects, short duration, and/or poorly controlled study design. For example, a recent study by Permut et al. showed positional therapy to be equivalent to CPAP at normalizing the AHI in patients with positional OSA.(4); however, this study was not blinded and did not evaluate the patients after the initial three study nights. Compliance with a positional device is problematic, with a compliance rate of 29% at 8 months in one study (5) and 6% at 2.5 years in another (6). Because of these issues, current practice parameters of the American Academy of Sleep Medicine recommend positional therapy as an effective secondary therapy or therapy that is supplemental to a primary treatment, particularly in individuals with “low AHI” (7). If positional therapy is utilized as a treatment modality, either as primary treatment, secondary treatment, or as supplemental therapy, it is imperative to document correction of OSA using an appropriate test (7) and maintain close clinical follow-up on a regular basis, particularly in light of decreasing compliance with positional devices over time.
Regarding the other choices in the question above, surgical evaluation for airway modification may be contemplated; however, surgery is often considered a second-line therapy in the treatment of OSA due to its associated morbidity and paucity of data regarding its efficacy (8). Although an oral appliance may be appropriate for this patient, oral appliances (OAs) are generally less efficacious than CPAP therapy, and there are conflicting reports about the performance of OAs in positional sleep apnea (9). While tracheostomy will effectively cure this patient’s OSA, it would not be considered an option in most patients unless the patient has suffered severe sequelae of untreated OSA and has exhausted all other treatment modalities.
Based on the above discussion, PAP therapy is the first-line treatment in the individual presented in the case. While CPAP is often the first choice of most clinicians, an auto-titrating device can be considered in this patient; the likely differential pressure requirements in the supine versus non-supine position in positional OSA may make this a more appropriate therapy, although this has not been shown in clinical trials at present.
References:
-
Chan AS, Lee RW, Cistulli PA. Non-positive airway pressure modalities: mandibular advancement devices/positional therapy. Proc Am Thorac Soc. 2008 Feb 15;5(2):179-84.
-
Yildirim N, Fitzpatrick MF, Whyte KF, Jalleh R, Wightman AJ, Douglas NJ. The effect of posture on upper airway dimensions in normal subjects and in patients with the sleep apnea/hypopnea syndrome. Am Rev Respir Dis. 1991 Oct;144(4):845-7.
-
Randerath WJ, Verbraecken J, Andreas S, Bettega G, Boudewyns A, Hamans E, Jalbert F, Paoli JR, Sanner B, Smith I, Stuck BA, Lacassagne L, Marklund M, Maurer JT, Pepin JL, Valipour A, Verse T, Fietze I; European Respiratory Society task force on non-CPAP therapies in sleep apnoea. Non-CPAP therapies in obstructive sleep apnoea. Eur Respir J. 2011 May;37(5):1000-28. Epub 2011 Mar 15.
-
Permut I, Diaz-Abad M, Chatila W, Crocetti J, Gaughan JP, D'Alonzo GE, Krachman SL. Comparison of positional therapy to cpap in patients with positional obstructive sleep apnea. J Clin Sleep Med 2010;6:238-243.
-
Wenzel S, Smith E, Leiacker R, Fischer Y. [Efficacy and longterm compliance of the vest preventing the supine position in patients with obstructive sleep apnea]. Laryngorhinootologie. 2007 Aug;86(8):579-83. German.
-
Bignold JJ, Deans-Costi G, Goldsworthy MR, Robertson CA, McEvoy D, Catcheside PG, Mercer JD. Poor long-term compliance with the tennis ball technique for treating positional obstructive sleep apnea. J Clin Sleep Med. 2009 Oct 15;5(5):428-30.
-
Morgenthaler TI, Kapen S, Lee-Chiong T, Alessi C, Boehlecke B, Brown T, Coleman J, Friedman L, Kapur V, Owens J, Pancer J, Swick T; Standards of Practice Committee; American Academy of Sleep Medicine. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006 Aug;29(8):1031-5.
-
Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, Harwick JD. Surgical Modifications of the Upper Airway for Obstructive Sleep Apnea in Adults: A Systematic Review and Meta-Analysis. Sleep. 2010;33(10):1396-1407.
-
Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara, W. Oral Appliances for Snoring and Obstructive Sleep Apnea: A Review. Sleep. 2006;29(2):244-262.