"The Air is Everywhere"
Abigail Strang, MD1 and Aaron Chidekel, MD1
Nemours/A.I. duPont Hospital for Children, Division of Pediatric Pulmonology
Wilmington, Delaware 19803, USA
Introduction:
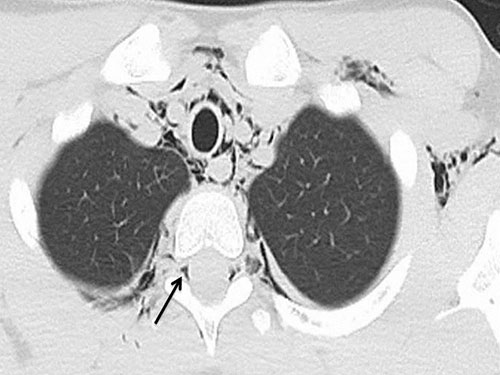
A 12-year-old male with a history of mild persistent asthma presented to the Emergency Department (ED) with acute onset of chest pain and a “crackling” feeling along his sternum. Two days prior he was seen by his pediatrician for coughing and wheezing associated with nasal congestion and sore throat. He was prescribed albuterol, prednisone, and azithromycin. In the ED, the patient had normal vital signs for age and a room-air oxygen saturation of 100%. On auscultation, lung exam showed diffuse end-expiratory wheezing. Crepitus was palpated in the neck, axillae, and along the sternum. The patient denied smoking or huffing, and there was no history of vomiting, strenuous physical activity, or trauma. A rapid respiratory panel was positive for Rhinovirus. A chest CT was obtained with findings as below:
Question:
Based on the chest CT findings, what are the best next steps in the management of this patient?
- MRI of the thoracic spine
- Medical management of bronchospasm with conservative management of air-leak syndrome
- Contrast esophagram
- Neurosurgical evaluation
Correct answer: B
Discussion:
The chest CT shows extensive pneumomediastinum with air extending from the pneumomediastium into the paraesophageal soft tissues, neck, axillae, and paraspinal soft tissues with a small amount extending into the spinal canal (pneumorrhachis). The patient was treated with bronchodilators and steroids for an acute asthma exacerbation and conservative medical management (bed rest, analgesia, oxygen) for pneumomediastinum. Symptoms and physical exam dramatically improved within 24 hours, and he was discharged home with close follow-up arranged.
Spontaneous pneumomediastinum is a rare condition that occurs when air enters the mediastinal cavity without a clear inciting event, such as trauma. This condition is most often seen in thin, young men who are smokers or in patients with underlying pulmonary disease (most commonly asthma). The most common presenting symptoms include chest pain and dyspnea1. The pathophysiology of spontaneous pneumomediastinum is thought to involve either the rupture of tracheobronchial or esophageal mucosal barriers, or alveolar rupture with resultant air escape into the respiratory interstitium with travel of air along a pressure gradient towards the mediastinum.2
Pneumorrhachis, which is usually found in conjunction with air collections in other body cavities, is defined as the presence of air in the intraspinal space. This rare condition is most often caused by trauma or iatrogenic causes (such as epidural anesthesia and lumbar puncture), but there are case reports of its association with pneumomediastinum associated with acute asthma exacerbations. In these cases, air likely tracks from the posterior mediastinum into the posterior epidural space, as there are no fascial barriers separating these structures.3
Although rare complications like pneumopericadium may occur, spontaneous pneumomediastinum generally follows a benign course with treatment of the underlying condition, rest, and analgesia.4 Similarly, in most cases of non-traumatic pneumorrhachis, the air resorbs spontaneously into the circulation over time.3 Although neurologic complications beyond mild headache are unlikely to occur, patients should be counseled to seek further medical care if they begin to experience neurologic deficits as more aggressive interventions may be warranted at that time.References:
-
Sahni S, Verma J, Grullon J, Esquire A, Patel P, Talwar, A. Spontaneous pneumomediastinum: Time for consensus. N Am J Med Sci 2013;5: 460-4.
-
Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944; 23: 281-358.
-
Manden PK, Siddiqui AH. Pneumorrhachis, pneumomediastinum, pneumopericardium and subcutaneous emphysema as complications of bronchial asthma. Ann Thorac Med 2009; 4: 143-5.
-
Macia I, Moya J, Ramos R, Morera R, Escobar I, Saumench J, Perna V, Rivas F. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothoracic Sug 2007; 31:1110-14.
-
Oertel MF, Korinth MC, Reinges MHT, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis, and management of pneumorrhachis. Eur Spine J 2006;15:S636-S643.



