Hole-y Moly
Erica Lin MD, Kenneth Chen MD, Grace Lin MD, Matthew Nobari MD
Division of Pulmonary and Critical Care Medicine and Department of Pathology
UC San Diego, La Jolla, CA, 92037, USA
Presentation:
A 32 year-old female with a past medical history of asthma presented to the emergency department for evaluation of an abnormal computed tomography (CT), initially obtained for hemorrhoidal bleeding. She reports a one-year history of gradually worsening shortness of breath and cough productive of yellow sputum. She is a current tobacco user and was previously employed as a smog technician. On physical examination, she had decreased air entry bilaterally. Laboratory studies were notable for ANA 1:80. Her chest imaging is shown below.
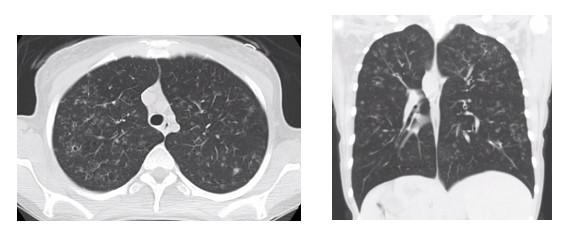
Figure 1: Axial (Left) and coronal (Right) images of CT chest
Question 1:
What is the likely diagnosis?
- Lymphangioleiomyomatosis (LAM)
- Birt-Hogg-Dube
- Pulmonary Langerhans Cell Histiocytosis
- Lymphocytic interstitial pneumonia
Question 2:
Which of the following is the best initial treatment?
- Smoking cessation
- Corticosteroids
- Antibiotics
- Pirfenidone
Question 1:
C. Pulmonary Langerhans cell histiocytosis
Question 2:
A. Smoking cessation
Discussion:
The patient’s clinical and radiographic presentation is most consistent with Pulmonary Langerhans Cell Histiocytosis. Choice A, B, and D are incorrect based on the radiographic findings. High-resolution CT chest can help distinguish amongst these cystic lung diseases. For example, the CT findings in LAM (Choice A) typically show multiple uniform thin-walled round cysts diffusely.1 BHD (Choice B) presents with lentiform thin-walled cysts in a basilar distribution on imaging.2 The cysts in LIP (Choice D) are random in distribution, may contain internal structures, are often bordered by a vessel and can be accompanied by ground-glass opacities.2
Pulmonary Langerhans Cell Histiocytosis (LCH) is a rare lung disorder characterized by Langerhans cells. It was previously termed as eosinophilic granuloma of the lung or pulmonary histiocytosis X.3,4 Studies have debated whether PLCH is an abnormal reactive process or a cellular proliferative process.1,4 Isolated PLCH occurs in young adults and almost exclusively in smokers, suggesting a possible contributing factor.1,3–5 While it is usually limited to the lungs, extrapulmonary manifestations can occur and include bone lesions, diabetes insipidus and skin changes.5 The classic radiographic findings demonstrate bronchiolocentric nodular and reticular opacities and bizarre-shaped cysts of varying sizes in a mid-to-upper zone distribution with sparing of the costophrenic angle.1,4 Bronchoscopy with transbronchial biopsy shows Langerhans cells that stain positive for S-100 and CD1a and pigment-laden macrophages (Figure 2).1,3,4 The most important recommendation is smoking cessation, as cessation may result in stabilization or remission of disease.3–5
To return to our case, we did recommend tobacco cessation as an initial treatment. After a long discussion, she recently quit smoking. She will continue to follow-up with pulmonary and hematology to assess whether her symptoms improve with this conservative measure.
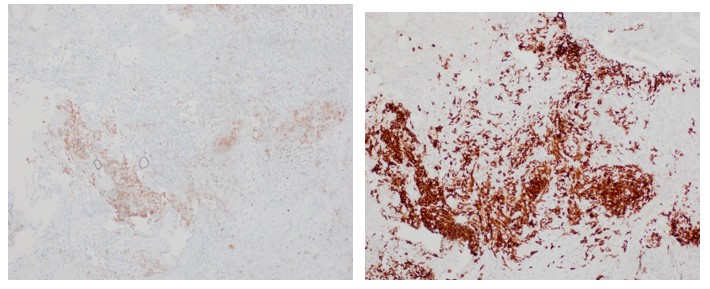
Figure 2: Langerhans cell with S100 (Left) and CD1a (Right) immunostaining in our patient
References:
-
Gupta N, Vassallo R, Wikenheiser-Brokamp KA, McCormack FX. Diffuse cystic lung disease: Part I. Am J Respir Crit Care Med. 2015;191(12):1354-1366. doi:10.1164/rccm.201411-2094CI
-
Gupta N, Vassallo R, Wikenheiser-Brokamp KA, McCormack FX. Diffuse cystic lung disease: Part II. Am J Respir Crit Care Med. 2015;192(1):17-29. doi:10.1164/rccm.201411-2096CI
-
Allen TC. Pulmonary Langerhans cell histiocytosis and other pulmonary histiocytic diseases: a review. Arch Pathol Lab Med. 2008;132(7):1171-1181. doi:10.1043/1543-2165(2008)132[1171:PLCHAO]2.0.CO;2
-
Suri HS, Yi ES, Nowakowski GS, Vassallo R. Pulmonary langerhans cell histiocytosis. Orphanet J Rare Dis. 2012;7(1):16. doi:10.1186/1750-1172-7-16
-
Tazi A. Adult pulmonary Langerhans’ cell histiocytosis. Eur Respir J. 2006;27(6):1272-1285. doi:10.1183/09031936.06.00024004



