Discovering Amelia Air-Heart
Authors: Savannah Ellis Knight, MD 1, Natalie Villafranco, MD 2
1 – Pediatric pulmonary fellow PGY-5, Baylor college of medicine and Texas Children’s Hospital
2 – Assistant Professor of pediatrics, division of pulmonary medicine, Baylor college of medicine and Texas Children’s Hospital
Case
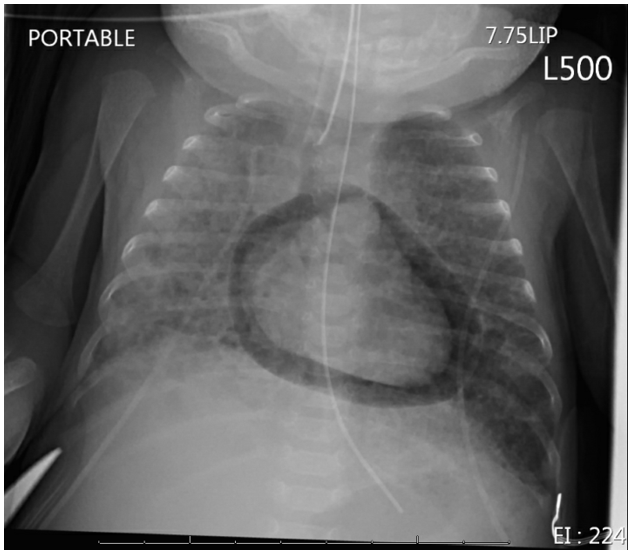
An 8-week-old former 28-week gestational age infant (corrected gestational age 36 weeks) with concern for developing bronchopulmonary dysplasia and pulmonary hypertension was admitted to the NICU. The infant was born prematurely for maternal pre-eclampsia and recently transferred from an outside institution intubated and requiring very high peak inspiratory pressures to reach tidal volumes that were adequate for his ventilation. His oxygen requirements included an FiO2 between 40-60% to keep his oxygen saturation greater than 90%, and a routine chest x ray to evaluate lung expansion and endotracheal tube positioning was obtained.
Question
What is this finding on the chest imaging?
- Pneumothorax
- Pneumomediastinum
- Pneumopericardium
- Pericardial effusion
C. Pneumopericardium
Discussion
The answer is C. pneumopericardium. Chest imaging shows a halo of air around the cardiac silhouette which is classic for pneumopericardium. It is caused by air from ruptured alveoli escaping into the interstitial spaces of the lungs and tracking through the conducting airways and into the pericardial sack via areas of weakness or embryonic connections between the pleura and pericardium. This phenomenon is similar to the “Macklin Effect” which describes how air from ruptured alveoli can travel along sheaths of pulmonic blood vessels into the mediastinum causing pneumomediastinum.
While not present in this case, pneumopericardium is usually associated with pneumothorax. Symptoms depend on the amount of trapped gas in the pericardium and can range from asymptomatic (only requiring supportive treatment) to sudden shock and tamponade physiology (requiring evacuation of air via pericardiocentesis). In our patient, the pneumopericardium was treated supportively with a change in ventilator settings including a decrease in PEEP, tidal volume, and inspiratory time. The pneumopericardium quickly resolved over the next 24 hours as mean airway pressures decreased.
An infant is diagnosed with bronchopulmonary dysplasia (BPD) when they are born before 32 weeks of age and require supplemental oxygen at 28 days of life. Our patient, who was a former 28-week infant with a corrected gestational age of 36 weeks and is requiring invasive ventilation with an FiO2 >30%, had grade 3, or severe BPD. BPD is characterized by alveolar simplification and abnormal vascular development, airway inflammation, injury and fibrosis that causes poor compliance of the lung parenchyma. However, in BPD, regional heterogeneity my be present with regions of the lung having differing airway resistance and compliance. For this reason, we can consider one mechanical ventilation strategy to optimize gas exchange in established BPD. This includes larger tidal volumes, longer inspiratory times, slower rates to allow for better emptying, and often higher positive end expiratory pressure (PEEP) to prevent dynamic airway collapse. Though air-leak in established BPD is rare, pneumopericardium is more likely in patients with underlying lung disease and those requiring invasive mechanical ventilation, as seen in our patient.
Pneumomediastinum is incorrect as it will appear on chest x-ray as lucency along not only the pericardium, but also around the entire mediastinum including the trachea, bronchi, and great vessels. Pneumothorax can be identified radiographically by the thin, white line of the visceral pleura separating the hyperlucent area from the rest of the lung. Pericardial effusion can be difficult to see from a chest x-ray and does no present with lucency.
References
-
Sprecher, Alicia J et al. “Pulmonary Air Leaks: Pneumothorax, Pneumomediastinum, Pulmonary Interstitial Emphysema, Pneumopericardium.” Nelson Textbook of Pediatrics. Twenty Second Edition. N.p., 2025. 1097-1098.e1. Web.
-
Jensen, Erik A et al. “The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-Based Approach.” American journal of respiratory and critical care medicine 200.6 (2019): 751–759. Web.
-
Abman, Steven H et al. “Interdisciplinary Care of Children with Severe Bronchopulmonary Dysplasia.” The Journal of pediatrics 181 (2017): 12-28.e1. Web.
-
Mosca, Fabio, Mariarosa Colnaghi, and Monica Fumagalli. “BPD: Old and New Problems.” The journal of maternal-fetal & neonatal medicine 24.S1 (2011): 80–82. Web.
-
Macklin, Charles. “Transport of Air Along Sheaths of Pulmonic Blood Vessels from Alveoli to Mediastinum: Clinical Implications.” Archives of Internal Medicine (1908) 64.5 (1939): 913-926. Web.