Blood in the Pleural Cavity
Prawin Kumar MD1, Nikhil Rajvanshi MD1, Kirtikumar J Rathod MCh2, Taruna Yadav MD3, Jagdish Prasad Goyal MD1, Pramod Sharma MD4
1Department of Pediatric, AIIMS Jodhpur, Rajasthan India
2 Department of Pediatric Surgery, AIIMS Jodhpur, Rajasthan India
3Department of Diagnostic and Interventional Radiology, AIIMS Jodhpur, Rajasthan, India
4 Department of Pediatrics, Dr. S.N. Medical College, Jodhpur, Rajasthan, India
Case
A 13-year-old male presented with sudden onset right-sided chest pain and difficulty breathing for seven days. Chest pain was diffuse, increased on deep inspiration, and associated with a dry cough but no fever. There was no significant past medical or family history. On examination, he had bilateral, non-tender swelling at the wrist, elbow, knee, and ankle joint with normal overlying skin. Respiratory examination revealed a bulging right hemithorax with decreased airflow. Trachea and PMI were shifted towards the left with reduced tactile fremitus on the right side. Air entry and vocal resonance were decreased on the right side with no adventitious sounds. Non-contrast CT chest was obtained, with the below findings:
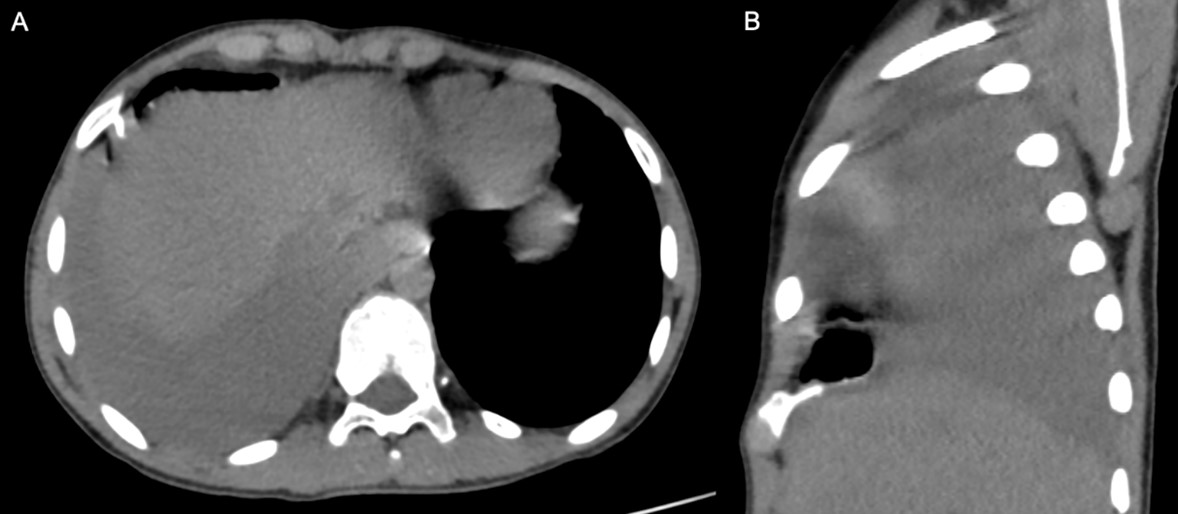
Figure 1. Non contrast CT scan showing high-density pleural fluid (33HU) on the right side. Bony exostoses from rib (red arrow).
Question 1
In addition to right-sided pleural effusion, what is the main abnormality in this image?
- Intrathoracic Mass
- Pneumomediastinum
- Bony Abnormality
- Pulmonary Embolism
Question 2
What is the next best step for management?
- Chest Tube Drainage
- Empirical Antibiotics
- CT Angiography
- Surgical Excision
Question 1 Answer
C. Bony Abnormality
Question 2 Answer
D. Surgical Excision
Discussion
Diagnostic work-up showed a normal hemogram (Hemoglobin 11.3 gm/dl; Total leucocyte count: 6620/cumm; Platelets: 5.27 lacs/cumm). The coagulation profile was also normal (INR: 1.16; Activated partial thromboplastin time: 29.6 seconds, Control: 27.8 seconds). Chest radiograph showed complete right-sided homogenous opacity with a mediastinal shift towards the left side. Ultrasound thorax showed a right-sided pleural effusion with increased echogenicity suggestive of hemothorax. A skeletal survey revealed multiple bony outgrowths originating in the juxta-epiphyseal region of long bones involving all four limbs. Computed tomography (CT) thorax showed bilateral bony outgrowths from ribs with right-sided hemothorax (Question-1). A diagnosis of multiple exostoses was made. Video-assisted thoracoscopic surgery (VATS) was performed on the right side with resection of rib exostosis and hemothorax evacuation. Histopathological examination of excised tissue was suggestive of osteochondroma. Clinical exome sequencing showed a heterozygous mutation in Exon 6 of the EXT1 (-) gene, establishing the diagnosis of Hereditary Multiple Osteochondromas/Exostoses (HMO/HME). The child did well on follow-up at one year with no recurrence of symptoms.
HME is an autosomal dominant skeletal disorder caused by a heterozygous pathogenic variant involving the EXT1 or EXT2 genes (1). It is characterized by multiple benign osteochondromas (exostoses) involving the metaphyseal region of long bones. The exact prevalence is not known. There is no gender predisposition; however, males tend to be more severely affected (2). Clinical features depend on the location of the exostoses. Clinical symptoms can occur due to osteoarticular complications like fractures, deformities, osteomyelitis, or compression of adjacent structures due to bony outgrowths, i.e., nerve or vascular compression. Positive family history is reported in most cases (1, 2). In approximately 10% of cases, de novo mutation occurs. The femur is the most common bone involved, followed by the tibia. Rib exostoses have been reported in approximately 35-45% of cases, which are primarily asymptomatic (3).
Hemothorax as a complication of HME is very rare and has been reported in only 15 patients. It has a male preponderance, with an average age of presentation being 11.7 years. Chest pain and shortness of breath are the most common symptoms, as in our index case (4). The estimated incidence of malignant degeneration to chondrosarcoma is around 2%-5%. Diagnosis can be established with chest radiographs and CT thorax in appropriate clinical settings. In cases where a normal chest x-ray results but there is a strong clinical suspicion, the patient must be evaluated with a CT thorax. Surgical treatment with resection of exostoses is the preferred treatment modality in symptomatic cases, VATS being the preferred approach (Question-2). In addition to acute management, resection of exostoses prevents the recurrence risk of hemothorax, establishes the histopathological diagnosis, rules out malignancy, and minimizes the risk of future malignant degeneration (5).
After resection, the estimated recurrence of exostoses is 2% in solitary osteochondroma during the pre-pubertal period. Recurrence in multiple exostoses has not been reported (4,5). More clarity regarding managing asymptomatic costal exostoses is needed. A conservative approach is mainly followed. The index case also had exostoses involving left hemithorax, for which no intervention was done. He remained well on follow up. Similarly, all asymptomatic osteochondromas remain symptom-free during follow-up in a case series by Bakshi H et al. (5). However, these patients must remain under close surveillance to look for any complications due to exostoses growth, especially during a pre-pubertal phase or malignant degeneration.
In conclusion, hemothorax is a rare complication of HME in children. CT scan is usually required to establish the diagnosis. Excision of rib exostoses in symptomatic children is the mainstay of treatment with an excellent outcome.
References
-
Funk ZM, Sharma PG, Carter CG. Hereditary Multiple Osteochondromas. Consultant. 2020;61(12):8–12.
-
Pedrini E, Jennes I, Tremosini M, Milanesi A, Mordenti M, Parra A, et al. Genotype-phenotype correlation study in 529 patients with multiple hereditary exostoses: identification of “protective” and “risk” factors. J Bone Joint Surg Am. 2011;93(24):2294–302.
-
Clement ND, Porter DE. Hereditary multiple exostoses: anatomical distribution and burden of exostoses is dependent upon genotype and gender. Scott Med J. 2014;59(1):35–44.
-
Sheaffer K, Hampton S, Barnard E, Patel MN, Kim L, Gendreau JL. Hemothorax and Pneumothorax Secondary to Costal Involvement in Hereditary Multiple Exostoses: A Systematic Review of Reported Cases in the Literature. Cureus. 2021;13(7): e16326.
-
Bakhshi H, Kushare I, Murphy MO, Gaynor JW, Dormans JP. Chest wall osteochondroma in children: a case series of surgical management. J Pediatr Orthop. 2014;34(7):733–7.



