The history of vomiting followed by sharp chest pain makes esophageal rupture secondary to transient increase in intra-abdominal and intraluminal esophageal pressure the most likely diagnosis. Pleural fluid amylase and amylase isoenzyme testing would be the best pleural fluid tests to confirm the diagnosis.
Pleural fluid amylase was 39,573 U/L and serum amylase was 122 U/L. Pleural fluid amylase greater than serum amylase may occur in a variety of clinical settings. Pleural fluid isoenzyme analysis is useful when the diagnosis is unclear. Predominantly pancreatic amylase is found in pancreatic diseases, such as acute pancreatitis and pancreatic pseudocyst. Predominantly salivary-type amylase occurs in esophageal rupture, malignant pleural effusion, ruptured ectopic pregnancy and rarely in parapneumonic effusion. Amylase levels in pleural fluid are elevated in all cases of esophageal rupture and are always of salivary origin (2).
Answer A is incorrect because pleural fluid lipase levels higher than serum lipase are seen in pleural effusions related to pancreatic disease, which is not consistent with the patient’s presentation. Answer B is incorrect because urinothorax typically presents as transudative effusion and does not fit the clinical scenario. Urinothorax is diagnosed by pleural fluid creatinine greater than urine creatinine. Finally, answers C and E are incorrect because pleural fluid triglyceride and cholesterol determination is helpful in diagnosing chylous and pseudochylous effusions, which are typically milky.
In the management of suspected esophageal rupture, it is important not only to confirm the presence of esophageal perforation but also to demonstrate the site of perforation for optimal management, including repair. The best method to determine the site of perforation is contrast esophagogram.
Barium contrast esophagogram is not the correct initial study because barium spilled into the mediastinum or pleural space elicits an inflammatory response and may obscure subsequent imaging studies (3). Because water soluble agents produce minimal inflammation and are rapidly absorbed, they are the preferred contrast agents in suspected esophageal rupture.
Diatrizoate meglumine (Gastrograffin) is the most commonly used water-soluble agent. However, water-soluble, nonionic, iohexol (Omnipaque) may be preferred to diatrizoate meglumine. Because of lower osmolality, iohexol is less likely to produce noncardiogenic pulmonary edema if aspirated into the lungs. However, all water-soluble agents are less opaque than barium so if suspected perforation is not demonstrated with a water soluble contrast agent, esophagogram with high-density barium is the next appropriate step (4).
In the present case, esophagogram with water-soluble contrast agent revealed leakage of contrast from the distal esophagus to the pleural space, confirming the diagnosis of esophageal rupture. The esophagogram with water-soluble contrast showing contrast in the distal esophagus, mediastinum, and pleura is shown in Figure 3.
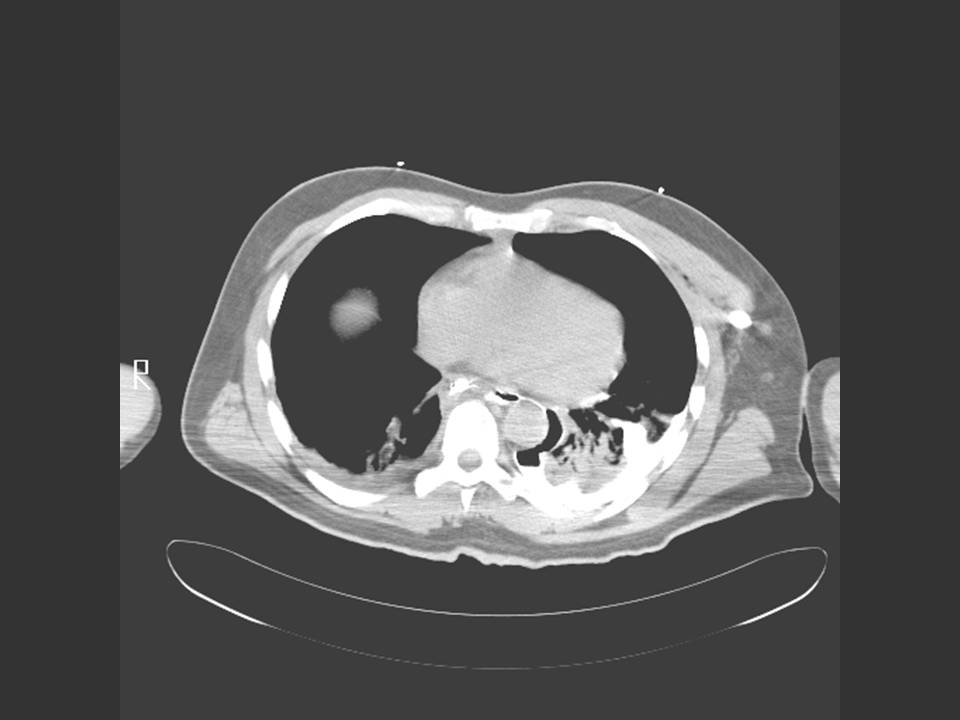
Chest CT is indicated if there is a high clinical suspicion of perforation but contrast esophagogram is negative. In addition, chest CT allows better delineation of the extent of mediastinal disease. Figure 4 shows leakage of contrast from the distal esophagus, across the mediastinum to the pleura.
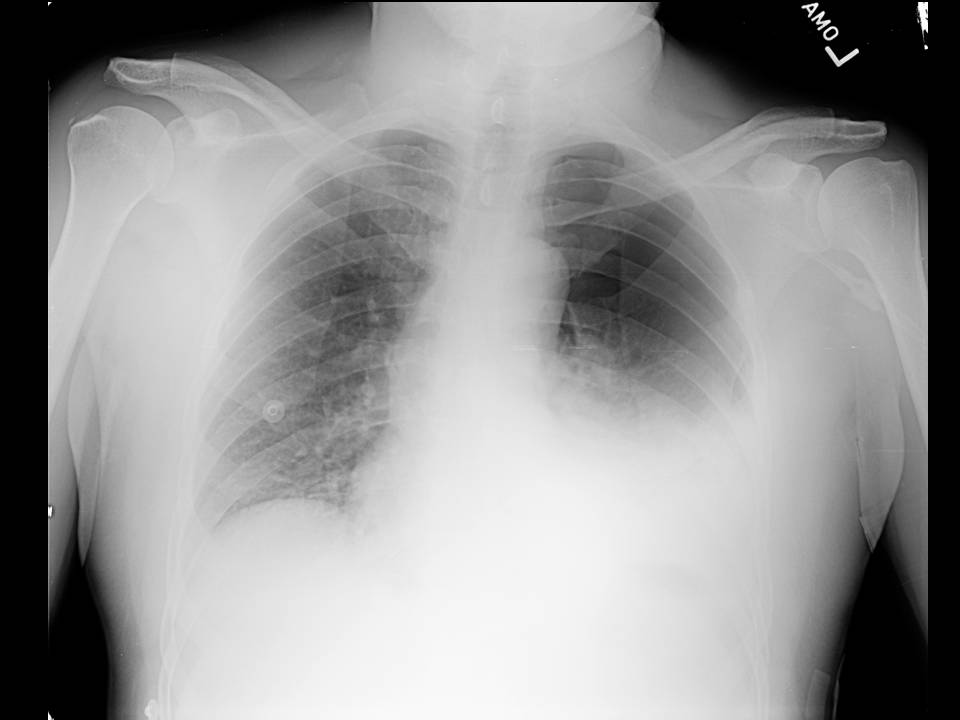
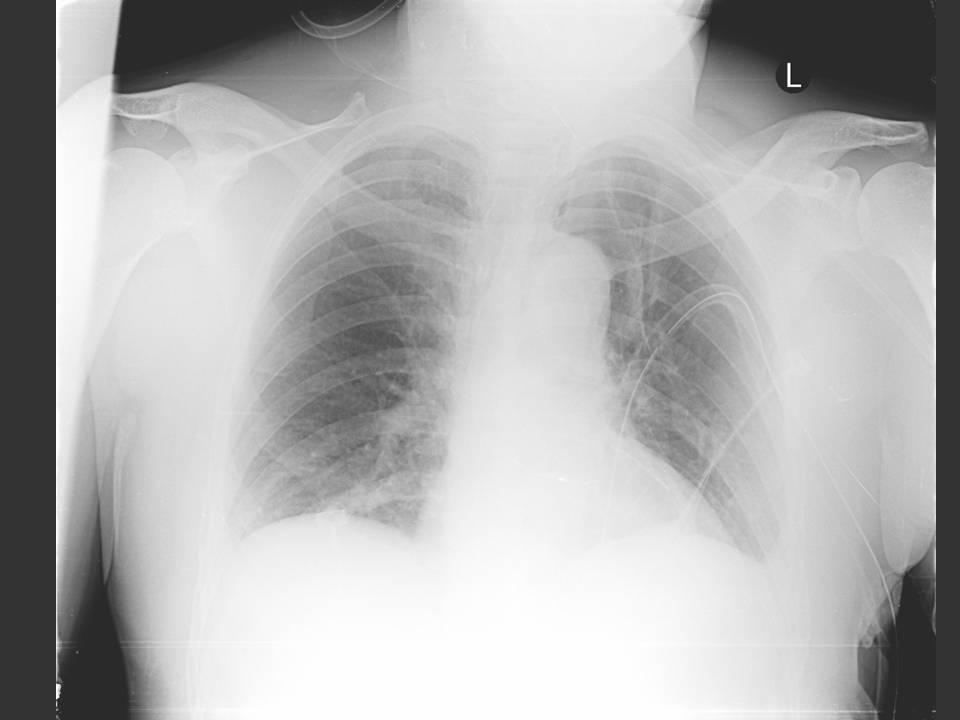
Ninety percent of spontaneous ruptures occur in the distal esophagus. Most occur on the left side just above the diaphragm, where the normal esophagus lacks serosal covering and there may be thinning of the muscularis mucosa. Seventy-five to 90% of spontaneous thoracic esophageal perforations are associated with left sided pleural effusions or hydropneumothorax, as seen in this patient (1).
Other radiographic findings seen in esophageal rupture include widening of the mediastinum, the presence of an air fluid level in the mediastinum, and in cases where the involved segment of esophagus is below the diaphragm, free air in the lesser sac or retroperitoneum may be seen (1).
The patient underwent thoracotomy with mediastinal and pleural drainage, repair of an 8 cm distal esophageal tear, open gastrostomy and placement of a feeding jejunostomy tube.
All patients with esophageal rupture require aggressive resuscitation and close monitoring. The vast majority of patients with esophageal rupture also require some form of surgery. The goal of any of the varied surgical approaches to esophageal rupture is to drain the infected mediastinum and pleura and eliminate ongoing contamination by repairing the disrupted site. Intrathoracic esophageal disruptions generally require aggressive mediastinal and pleural drainage via thoracotomy (5).
To limit ongoing mediastinal contamination and permit healing in the peri-operative period, cessation of further oral intake, gastric decompression, and broad-spectrum antibiotics are indicated (5). Answer A is the only answer that addresses all aspects of elimination of ongoing contamination, drainage of infected mediastinum and pleura as well as peri-operative healing.
Iatrogenic instrumentation is the most common cause of esophageal perforation but is associated with the lowest mortality rates for perforation (6). The improved outcome in these patients is multi-factorial: (1) early presentation since they are already in a monitored, health care setting, (2) NPO status eliciting a milder inflammatory response, (3) cervical esophageal perforations tend to have a more benign course.
Postemetic rupture of the esophagus, initially described by Boerhaave in 1724, usually requires surgery. Operative management of such ruptures more than 24 hours after the initial injury had previously been considered controversial, due to high mortality in this subgroup (7). However, more recent data suggest that repair of intrathoracic esophageal perforation is preferred to nonoperative management, regardless of the duration of injury provided there is no cancer or irreversible distal obstruction (8).
Nonoperative management of postemetic esophageal rupture may be indicated when the rupture is confined to the mediastinum. Patients with a contained rupture are less likely to be symptomatic and often remain clinically stable. However, before committing to a nonoperative approach, the time interval from injury should be sufficiently long for the patient to manifest signs and symptoms of uncontained rupture (5). Patients with corrosive injuries invariably require surgery and often require resection rather than repair.
Answer E is correct because this is the only option of a clinical scenario in which the rupture is likely confined to the mediastinum and has been observed for a long enough period of time to verify that the rupture is asymptomatic.
The patient described in this clinical case had an uncomplicated postoperative course, tolerating tube feeds by postoperative day 4. A repeat esophagogram demonstrated no leak of water-soluble contrast and the patient was discharged home on postoperative day 10.