Reviewed By Pulmonary Circulation Assembly
Submitted by
Sugeet Jagpal, MD
Fellow
Division of Pulmonary and Critical Care Medicine
Rutgers University Robert Wood Johnson Medical School
New Brunswick, New Jersey
Vyacheslav Gendel, MD
Division of Interventional Radiology
Rutgers University Robert Wood Johnson Medical School
New Brunswick, New Jersey
John L. Nosher, MD
Division of Interventional Radiology
Rutgers University Robert Wood Johnson Medical School
New Brunswick, New Jersey
Lakshmi Uppaluri, MBBS
Assistant Professor
Department of Pediatrics
Rutgers University Robert Wood Johnson Medical School
New Brunswick, New Jersey
Submit your comments to the author(s).
History
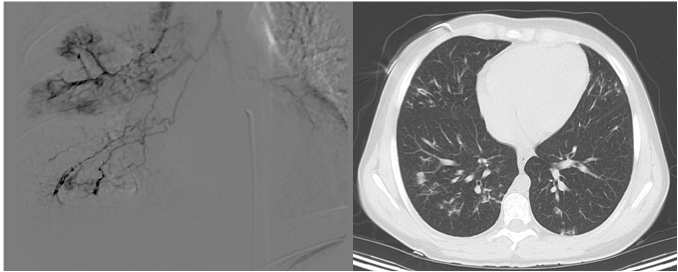
A Caucasian child had Cystic Fibrosis (CF) diagnosed at birth with a positive sweat chloride test, and required surgery as a neonate for meconium ileus. A liver biopsy at three months of age demonstrated focal biliary cirrhosis, and the patient suffered from esophageal varices that required sclerotherapy until eighteen months of age. From the age of two onwards the patient did not have further clinical manifestations of cirrhosis. Her pulmonary symptoms were not significant, and imaging demonstrated mild bronchiectasis of the right middle and lower lobes. Genotyping was done during adolescence, and she was found to have one copy of ΔF508 while the second mutation remained unknown.
After being lost to follow up for several years, the patient presented to our emergency room at the age of seventeen with nausea and dizziness.
Physical Exam
The vitals on admission revealed mild sinus tachycardia with a pulse of 90/minute, systolic blood pressure between 90-100 mm Hg range, but no tachypnea, pain or fever. Exam demonstrated a thin female who was developmentally normal for her age. She did not have any overt manifestations of cirrhosis, with no spider angiomas, palmer erythema, or asterexis noted. Her lung exam was positive for mild crackles at the right lung base, and she did not have clubbing. Abdominal exam was benign with normoactive bowel sounds.
Orthostatics were attempted and rapidly aborted when the patient vomited a moderate amount of bright red blood. Blood work demonstrated that her hemoglobin and platelets had decreased compared to prior labs (9 gm/dl Hg and platelets 100,000/ µL), and she was admitted to the pediatric intensive care unit. She was given packed red blood cells, esomeprazole and octreotide drips were administered, and endoscopy was planned.
References
- Rowland M, Bourke B. Liver disease in cystic fibrosis. Current Opinion in Pulmonary Medicine 2011; 17:461-466
- Cheng K, Ashby D, Smyth RL. Ursodeoxycholic acid for cystic fibrosis-related liver disease. Cochrane Database Systemic Review 2012; Issue 10
- Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med 2000;28:1642-1647
- Funaki B. Systemic arterial embolization for hemoptysis. Seminars in Interventional Radiology 2010; 314-319.
- Schnader J, Smith R, Britt EJ, Katz A, Kelley M, Schraufnagel D. Hemoptysis, Hepatopulmonary Syndrome, and Respiratory Failure: Clinical Conference on Management Dilemmas. Chest 1997; 111:1724-32
- Fritz J, Fallon M, Kawut, S. Pulmonary vascular complications of liver disease. Am J Respir Crit Care Med 2013;187: 133–143